Snoring & Sleep Apnea Surgery
What is obstructive sleep apnea (OSA)?
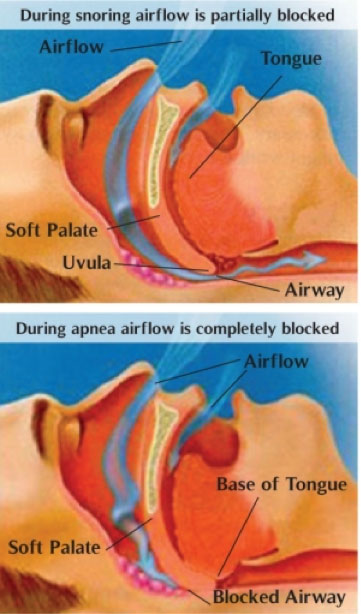
The most common type of sleep apnea is obstructive sleep apnea. During sleep, enough air cannot flow into your lungs through your mouth and nose even though you try to breathe. When this happens, the amount of oxygen in your blood may drop. Normal breaths then start again with a loud snort or choking sound.
When your sleep is upset throughout the night, you can be very sleepy during the day.
With sleep apnea, your sleep is not restful because:
- These brief episodes of increased airway resistance (and breathing pauses) occur many times.
- You may have many brief drops in the oxygen levels in your blood.
- You move out of deep sleep and into light sleep several times during the night, resulting in poor sleep quality.
People with sleep apnea often have loud snoring. However, not everyone who snores has sleep apnea.
Some people with sleep apnea don’t know they snore:
- Sleep apnea happens more often in people who are overweight, but even thin people can have it.
- Most people don’t know they have sleep apnea. They don’t know that they are having problems breathing while they are sleeping.
- A family member and/or bed partner may notice the signs of sleep apnea first.
Untreated sleep apnea can increase the chance of having high blood pressure and even a heart attack or stroke. Untreated sleep apnea can also increase the risk of diabetes and the risk for work-related accidents and driving accidents.
Our doctors at C/V ENT Surgical Group, serving the Los Angeles and Thousand Oaks areas, are experts in the diagnosis and treatment of snoring and sleep apnea. They will start with obtaining a thorough history of your concerns and symptoms and subsequently perform a workup to diagnose the cause of your sleep disorder.
Once a diagnosis is reached, whether this may be simple snoring or severe obstructive sleep apnea(OSA), they can guide you regarding which treatment options may be best to help you obtain restful sleep not only for you but also for your bed partner. These options are detailed below and they include various procedures including in-office procedures with minimal downtime to more invasive surgical procedures.
What causes sleep apnea?

This happens if the following conditions occur:
- Your throat muscles and tongue relax more than is normal.
- Your tonsils and adenoids are large.
- Your nose is obstructed due to a deviated septum, large turbinates or nasal polyps.
- You are overweight.
- The extra soft tissue in your throat makes it harder to keep the throat area open.
- The shape of your head and neck (bony structure) results in somewhat smaller airway size in the mouth and throat area.
- You have a very floppy palate with a thick or long uvula.
- You have a very large base of tongue that flops back and blocks your breathing.
With these areas in your nose and throat being partly blocked during sleep, enough air cannot flow into your lungs, even though your efforts to breathe continue. Your breathing may become hard and noisy and may even stop for short periods of time (apneas).
Another rare type of sleep apnea, termed central sleep apnea, happens when the area of your brain that controls your breathing doesn’t send the correct signals to the breathing muscles. Then there is no effort to breathe at all for brief periods. Snoring does not typically occur in central apnea and is not treated by our surgeons.
Who is at risk for obstructive sleep apnea (OSA)?
Anyone can have obstructive sleep apnea. It is estimated that more than 12 million Americans have obstructive sleep apnea. More than half the people who have sleep apnea are overweight, and most snore heavily.
Sleep apnea is more common in men. One out of 25 middle-aged men and 1 out of 50 middle-aged women have sleep apnea that causes them to be very sleepy during the day. Sleep apnea is more common in African Americans, Hispanics, and Pacific Islanders than in Caucasians. If someone in your family has sleep apnea, you are more likely to develop it than someone without a family history of the condition.
Adults who are most likely to have sleep apnea:
- Snore loudly.
- Are overweight.
- Have high blood pressure.
- Have a decreased size of the airways in their nose, throat, or mouth. This can be caused by the shape of these structures or by medical conditions causing congestion in these areas, such as hay fever or other allergies.
- Have a family history of sleep apnea.
Obstructive sleep apnea can also occur in children who snore. If your child snores, you should discuss it with our physicians.
What are the symptoms of obstructive sleep apnea (OSA)?
The most common signs of sleep apnea are:
- Loud snoring
- Choking or gasping during sleep
- Fighting sleepiness during the day (even at work or while driving)
Your family members may notice the symptoms before you do. Otherwise, you will likely not be aware that you have problems breathing while you are asleep.
Others signs of sleep apnea may include:
- Morning headaches
- Memory or learning problems
- Feeling irritable
- Not being able to concentrate on your work
- Mood swings or personality changes perhaps feeling depressed
- Dry throat when you wake up
- Frequent urination at night
How is obstructive sleep apnea (OSA) diagnosed?
Your doctors will do a physical exam, take a medical history that includes asking you questions about how you sleep and how you function during the day and have you fill out a detailed questionnaire that will risk-stratify you in relation to your snoring and sleep apnea. As part of the exam, your doctor will check your mouth, nose, and throat to determine areas of obstruction. For example, a deviated spetum, large turbinates, enlarged tonsils, a long or thick uvula (the tissue that hangs down in the middle in the back of your throat), a floppy soft palate or a large base of tongue. Your doctor may order a sleep recording if your symptoms are severe enough based on your history, exam and questionnaire results to grade your sleep apnea into mild, moderate or severe types.
What are the treatment options for snoring and obstructive sleep apnea?
Continuous positive airway pressure (CPAP) is the most common treatment for moderate to severe sleep apnea and is the gold standard for treatment, however many people cannot tolerate use of this cumbersome mask and machine. For this treatment, you wear a mask over your nose during sleep. The mask blows air into your throat at a pressure level that is right for you. The increased airway pressure keeps the throat open while you sleep.
If you are one of the many who cannot tolerate CPAP for one reason or another and you have mild to moderate sleep apnea you may be a candidate for one of the surgical treatment options the physicians at C/V ENT Surgical Group in Los Angeles utilize listed below, which include in-office procedures.
Pillar Implant Procedure
The revolutionary Pillar procedure, or palatal implants, is a new and minimally invasive modality approved by the FDA and is used to treat people with habitual snoring and those with mild-to-moderate OSA with excellent results. The Pillar procedure addresses the soft palate, which is one of the main anatomic components of sleep apnea and snoring. During the Pillar procedure, 3 to 5 tiny woven inserts are placed in the soft palate to help reduce the vibration that causes snoring and the ability of the soft palate to obstruct the airway.
Once in place, the inserts add structural support to the soft palate. Over time, the body’s natural tissue response to the inserts (which are made of nothing more than suture material that is used in everyday surgery) increases the structural integrity of the soft palate. This procedure is performed in the office under local anesthesia and usually takes about 30 minutes. One can return to normal eating and function the same day. Results, however are not seen until 2-4 months after the procedure when the palate has stiffened due to the normal scarring process.
A study performed in Norway indicated that the procedure is successful (70%) in terms of bed-partner satisfaction (Nordgard, 2006). The cure rate for sleep apnea depends on the severity of the preoperative level of sleep apnea. However studies have shown it is 80-90% effective as a treatment for snoring.
Our surgeons at C/V ENT Surgical Group, which serves the Los Angeles and Thousand Oaks areas, are now utilizing this procedure with great results. Sometimes they perform this procedure in combination with a coblation assisted uvulectomy to target both the anterior and posterior soft palate in patients with a large uvula. Note that laser uvulectomy, if performed, does add a moderate amount of post-procedural pain and discomfort to the in-office procedure.
The pillar implant procedure was recently highlighted on “The Doctors” and can be seen here:
Laser Assisted Uvulopalatoplasty (LAUP)
This is a procedure utilized by the surgeons at C/V ENT Surgical Group in addition to the pillar implant procedure or as a standalone procedure in appropriate candidates as a treatment for snoring and mild to moderate sleep apnea. During this in-office procedure a rim of soft palate containing the uvula is removed using the laser. In the past the laser used was the CO2 laser which was associated with significant pain for up to 2 weeks following the procedure.
However our physicians now utilize the cold laser or radiofrequency energy (aka Coblation) to obtain the same result with significantly less discomfort which consists of a mild to moderate sore throat for approximately one week. Most patients state that the discomfort is manageable and after 24-48 hours they can resume normal activities, although a soft diet is recommended for one week.
In carefully selected patients this procedure as a stand alone procedure or in combination with the pillar implant procedure can provide tremendous improvement in snoring and sleep apnea symptoms. Call our surgeons serving the Los Angeles and Thousand Oaks areas to schedule a consultation to discuss if you are an appropriate candidate for this revolutionary procedure.
Coblation
This includes a number of procedures which utilizes radiofrequency energy to ablate excess soft tissue whether this is in the nose (turbinates) or in the throat (base of tongue, soft palate, uvula, or tonsils). Our surgeons, serving the Los Angeles and Thousand Oaks areas, are experts in the utilization of coblation to address areas of obstruction such as in turbinate reduction surgery, tongue base reduction surgery, tonsil reduction surgery, soft palate stiffening surgery, or laser uvulectomy.
Tonsillectomy and Adenoidectomy
When children under the age of 13 are diagnosed with severe snoring or obstructive sleep apnea, this is often due to enlarged adenoids and tonsils. As a result these children would benefit from adenoidectomy and tonsillectomy if warranted by their history and physical exam. Our surgeons at C/V ENT Surgical Group, which serves the Los Angeles and Thousand Oaks areas, routinely perform tonsillectomy and adenoidectomy in children and young adults with severe snoring and obstructive sleep apnea. Many parents will return months after the procedure and report that their children are much more calm and doing better at school since they are now getting restful sleep nightly.
Uvulopalatopharyngoplasty (UP3/UPPP)
Uvulopalatopharyngoplasty (UP3/UPPP) in general is the most common and oldest procedure for the treatment of obstructive sleep apnea (OSA) in the United States. This procedure, introduced by Fujita in 1981, consists of tonsillectomy, reorientation of the anterior and posterior tonsillar pillars, and excision of the uvula and posterior rim of the soft palate. This is quite an invasive procedure that entails a general anesthetic and involves removal of the tonsils, uvula, and part of the soft palate. In some patients, however, with moderate to severe OSA who cannot tolerate CPAP it is necessary.
The hardest part is not the surgery itself, but the recovery from this procedure. There is significant pain for 7-15 days, as the area in the back of the throat heals, requiring pain medication regularly and a liquid or soft diet for that period. This procedure is at times combined with tongue base reduction surgery when indicated. Our surgeons perform uvulopalatopharyngoplasty (UP3/UPPP) in patients with moderate to severe obstructive sleep apnea that are noted on exam to be good candidates and have failed CPAP treatment.
Tongue Base Reduction
This is a procedure often used in combination with other procedures when a patient is in the operating room. The most common method used by our physicians to treat a large base of tongue is to use coblation. In this procedure, radiofrequency energy is used via a coblation wand to target 3 to 4 points within the base of tongue and subsequently shrink them. The results are seen over months as the tissue heals and scars causing some reduction in bulk.
Septoplasty
This is one of the most common procedures performed to improve nasal obstruction when necessary. The septum is made of bone and cartilage and is the dividing wall between the two nasal passages. Often times it can be deviated to one side or another causing unilateral obstruction or be S-shaped causing bilateral obstruction in patients.
One may be born with these deviations or it can be acquired due to nasal trauma. During a septoplasty no cuts are made on the face but a small incision is made inside the nose and the deviated portions of cartilage and bone are either removed or straightened in order to improve nasal congestion. Often times our doctors combine this procedure with turbinate surgery to significantly enlarge the nasal airways and improve your breathing.
These procedures do not affect the shape and look of your nose as they are functional surgeries on the inside of your nose. However, some patients would like cosmetic changes made to their nose via a rhinoplasty at the same time and this can be accommodated to by our surgeons at your consultation. These changes include dorsal hump removal, fixing a crooked or deviated nose or tip refinement. The surgeons at C/V ENT Surgical Group, which serves the Los Angeles and Thousand Oaks areas, are renowned head and neck and facial plastic surgeons, who perform septoplasty (deviated septum repair) routinely with outstanding results.
Submucous Resection of Inferior Turbinates
The turbinates are curved ridges along the sidewall of the nose on each side and are involved in humidification and filtration of the air we breathe in. There are 3 sets of turbinates on each side of the nose. The most inferior set is responsible for nasal congestion and is termed the inferior turbinates. There are various types of turbinate surgery. There are in-office options with radio frequency ablation of the inferior turbinates (Coblation) that help shrink the mucosa of the turbinates and sometimes require more than one treatment for results.
Then there are more definitive procedures such as submucous resection of the turbinates that are performed under anesthesia. During this procedure the bone expanding the turbinates on the inside is shaved down allowing for significant long-term reduction in the size of the turbinates. Often times this procedure is combined with a septoplasty/deviated septum repair when necessary to significantly improve nasal obstruction. Our surgeons in Los Angeles and Calabasas will accurately assess the cause of your nasal obstruction and determine if turbinate surgery will significantly improve breathing through your nose.
